Does strength training help with osteoarthritis? Or does exercise actually make the joint disease worse? We looked at the science behind the risk factors for osteoarthritis and found results - from prevention to alleviating symptoms (including suitable exercises for osteoarthritis).
A stabbing pain in the hip or knee, restricted movement or even stiffness in the hands: Osteoarthritis can manifest itself through many different symptoms. Particularly after prolonged exertion such as jogging or standing for too long, when unscrewing a jam jar or even when climbing stairs, sufferers feel the pain in their joints. And they are not alone: Osteoarthritis is one of the most common joint diseases worldwide. According to the RKI, almost half of women (48.1 %) and just under a third of men (31.2 %) aged 65 and over were affected in Germany in 2017 (1). And although the disease is so widespread, many people still wonder: How does osteoarthritis develop and what helps with symptoms? We take a closer look at strength training in particular. Because there are some myths surrounding osteoarthritis. We have also prepared a short training plan for osteoarthritis.
What is osteoarthritis?
Osteoarthritis is a joint disease in which the joint cartilage is damaged and degraded. This wear and tear puts excessive strain on the bones and various changes take place around the bone. These can be, for example, a thickening of the bone plate, calcification of the joint capsule or inflammatory reactions. The joints of the hip, knee or hand are most frequently affected, but the spine can also suffer from wear and tear.
Risk factors for osteoarthritis
As the first symptoms often occur during exercise, movement and sport, especially intensive units such as strength training, are quickly demonised and avoided. After all, the joints should be spared. Sport is also sometimes cited as a risk factor for osteoarthritis. However, both theories are a false assumption. The truth is that the development of the disease is complex and very different factors can favour osteoarthritis:
- Hormones and genetic factors: Women are more frequently affected due to menopause, for example
- Injuries and excessive strain that damage the joint cartilage: These can be fractures, knocks, bruises or incorrect loading over the years, but excess weight also plays a role
- Untreated malpositions
Current research is increasingly showing that an incorrect diet and, in particular, a lack of exercise also promotes the development of osteoarthritis. So instead of demonising sport, exercise should play an important role for healthy joints and cartilage.
Does strength training lead to premature osteoarthritis?
Even if excessive, incorrect strain over many years is considered a risk factor for osteoarthritis, strength training does not generally lead to osteoarthritis. On the contrary: regular strength training can prevent arthritic complaints. However, three aspects are very important in order not to harm your body and to minimise the risk of injury:
- Intensity and frequency must not be increased too quickly during strength training
- Adequate rest periods are important and must not be neglected
- On the other hand, too little exercise or even inactivity does not lead to a positive change in the human body.
As in many areas of life, the dose is the key to success. So if you dose correctly and carry out your strength training with adequate load and rest phases, you reduce the risk of premature osteoarthritis rather than promoting the disease.
Is strength training good for existing osteoarthritis?
Patients who are already suffering from osteoarthritic symptoms should integrate a healthy amount of strength training into their daily routine just as much as people who want to prevent osteoarthritis. There is increasing and very good scientific evidence for this, e.g. reviews on the subject of "Strength training/training therapy for osteoarthritis". They all show that Strength training provides significant relief in terms of pain and everyday limitations. The assumption that an osteoarthritic joint is "worn out, used up, broken or unable to bear weight" and should therefore not be trained is not true. Customised training therapy can also help with severe forms of osteoarthritis.
Our bodies are capable of learning and change at every age. When we exercise, our cartilage, bones, tendons and muscle structures adapt. They try to adapt to the regular mechanical stress. Don't you think so? Then just take a look at athletes in different disciplines. They show impressively that stimuli really do trigger adaptation mechanisms. Depending on the discipline, strong structural differences can be recognised. For example, weightlifters have a different cartilage structure in their joints than a footballer. The body adapts to its load.
Training plan for osteoarthritis
Overall, we can only advise you to do so: Get started with strength training. We will be happy to help you set up a suitable training programme. And to help you get started now, we have put together an initial training programme for osteoarthritis.
Our training programme is specially designed for knee and hip osteoarthritis and is based on the "NEuroMuscularExercise training programme". This involves strength, stability and movement-enhancing exercises. The following is very important for all exercises: pay attention to your personal pain level during and after the exercise.
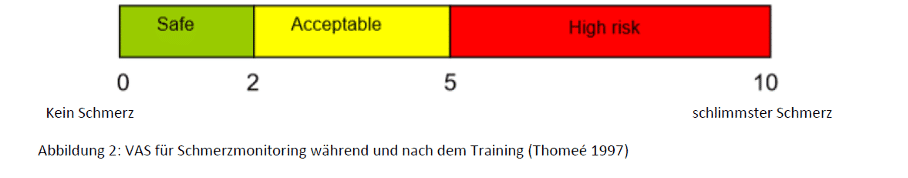
If you feel pain during the exercises that goes far beyond your usual level, reduce the intensity. For example, think of your pain on a scale of 1 to 10, where 0 is no pain and 10 is the worst pain. Between 2 and 5 can be considered safe and acceptable, depending on your ability to cope. However, do not go beyond 5. The pain should also subside to its "normal" level the day after training.
Otherwise, the same applies to all exercises:
- 2-4 sets
- 8-20 repetitions (depending on load capacity)
- At least 1 minute break after each set
The exercises can be completed in the form of circuit training or one after the other.
Warm up:
- 10 min. bicycle ergometer (individual watt load) up to a pulse rate of 120/min
- Goal: easy effort
Exercises for training:
- Pelvic lift with or without Pezziball; increase by extending the lever or on one leg
- Sit-ups with or without Pezziball; increase by extending the lever
- Slide exercises: Slide a towel forwards, backwards, sideways; increase with unstable support surface
- Box squat, squat or box squat on one leg (squats): Increase by placing the leg to be trained backwards, so-called "lunges"
- Step up/step down: Increase through higher level
- Functional leg press (single leg)
- Knee extension machine/Theraband (single leg)
- Knee flexor machine/Theraband (single leg)
Cooling down and stretching:
- Heel stretch: support the knee with a cushion
- Squat stretch hold on a bar
- Extension stretching with fascia roll, e.g. Blackroll